Breastfeeding in the NICU
We understand that feeding can bring up a lot of emotions for parents. We want to make sure you have all of the information about breastfeeding to help you make an informed decision with your baby’s NICU team.
“Liquid Gold”
Your breastmilk is the optimal food for your baby. It’s made to meet your baby’s specific needs.
Benefits of breastfeeding for babies in the NICU:
- Fewer infections
- Better digestion
- Helps with brain development
- Helps your baby go home sooner
Benefits of breastfeeding for the mother:
- Increases bonding to your baby
- Better coping during this stressful time
- Less risk of breast cancer
Depending on your baby’s needs, there are 3 ways your baby may feed your breastmilk:
- At the breast
- Through a feeding tube
- With a bottle
The BEST way to make lots of breastmilk is to start hand expressing frequently as soon as the baby is born.
Golden rules
- Start hand expressing early. Ideally, within 1-2 hours after birth. Express for 10-20 minutes every 3 hours. Start as soon as you can. It’s never too late!
- Every drop counts. Do not throw away any breast milk. Drops are normal. Collect them in a syringe and have someone bring them to your baby. Even if there are no drops, continue to stimulate regularly.
- Express 8 times each day. First, start with hand expression then add in a breast pump.
All about pumping
Manual expression
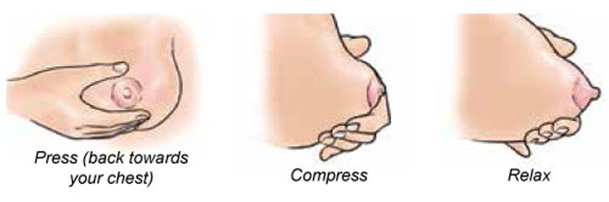
- To get milk to flow, start by massaging your breast gently for 1-2 minutes.
- Make a “C” with your thumb and index finger.
- Place your thumb and your index finger on either side of the nipple, 2 to 5 cm away.
- Press your fingers into your breast by pushing back into your ribs.
- Bring your thumb and index finger together. You do not need to press hard.
- Repeat the motion several times, repeating the same rhythmic movements.
- Do not slide your fingers along your breast.
- Maintain firm pressure on your breast without stretching the nipple.
- Work your way around the breast with your fingers until it is emptied.
Collect drops into a medicine cup. Once all of the drops are in a cup, you can then suck them into a syringe to store.
Expressing with a breast pump
The time has come to add a breast pump to your breastfeeding routine. Here are the steps to follow:
- Wash your hands before pumping
- Pump 8 times per day, including at least once overnight (between 00:00 and 05:00) to establish good milk production
- Before your milk comes in, pump each breast for 15 minutes. (You can pump both breasts at the same time or one at a time). Once your milk is in, pump until breasts are “emptied” (until very low milk flow).
- Breast milk must be put in syringes or bottles provided by the hospital.
- Put a sticker with your baby’s name on each bottle. Write the date and the time the milk was pumped. Ask for stickers at the front desk of the NICU
- If you are sick (cold, flu, gastroenteritis, COVID-19) your baby still needs your milk. It will provide antibodies, which protect against infection.
Cleaning your pump kit
Clean after each use. Take your kit apart in the bowl or basin given. Wash each piece with hot soapy water (no soaking). Do not wash tubing. Do not leave the tubing on or in the pump when you leave the NICU.
Disinfect your kit once a day. Boil in water for 5-10 minutes or place in the dishwasher or use a pump sterilizing bag in the microwave. A microwave for pump kit disinfection is available in the NICU.
Transportation and storage of breast milk
- Fresh or refrigerated breast milk must be put in the refrigerator outside the milk lab in the NICU. Place it in the bin with your baby’s name.
- When you bring milk from home, use an insulated lunch bag or cooler with an ice pack.
- At home, put your milk in your refrigerator. If your milk is at home for more than 24 hours, please freeze.
- Frozen milk must stay frozen on your way to the hospital and must be placed in the milk lab freezers when you arrive. Our freezer space is limited so please plan to store some frozen milk at home.
- Breast milk can be kept for 6-12 months in a freezer.
Pumping videos
- Manual expression of breastmilk – YouTube
- Using the breast pump – YouTube
- Maximizing breastmilk production – YouTube
- Milk storage and pump kit cleaning – YouTube
FAQs on breastfeeding
#1 – Do I need to express my milk?
Yes! Babies in the NICU will not be able to breastfeed right away. If you express drops of breastmilk starting 1-2 hours after birth, you will have better milk supply in the long term. If you do not express breastmilk early, your body will not know that it needs to make milk.
#2 – Do I have access to a breast pump at the hospital?
Yes. You can ask your postpartum nurse to bring you a breast pump to your room after giving birth. Remember to ask for help with expressing milk with your hands as soon as possible. There is also always a pump in your baby’s NICU room. A NICU nurse will give you a kit for hand expression and to use with a pump.
#3 – Do I need a breast pump at home?
Yes. You need to pump 8 times every 24 hours so you will need a pump at home. An electric breast pump is better than a manual pump.
You can purchase or rent a pump at stores that sell breastfeeding supplies (e.g. Walmart, Melon and Clémentine) or buy online. There are organizations that can help you (e.g. Entre Maman et Papa, Préma-Québec). Do not buy a used pump (think of it like a toothbrush!).
The cost to rent is usually ~$90 per month. A refundable credit card deposit is usually required. The cost to buy a pump is usually $200-300 for a single pump (pump one breast at a time) or $350-450 for a double pump (pump both breasts at the same time).
#4 – Are there reasons why someone should not breastfeed?
Breastfeeding contraindications are rare. Even if you are sick, your baby still needs your milk, and your milk helps to prevent infection. It is safe to breastfeed while taking most medicines because only a small amount ends up in your breastmilk. If you have questions about any medicine, breastfeeding consultants and pharmacists are here to help.
#5 – If I had breast surgery (reduction or augmentation), will I still be able to make milk?
You can still make milk by following the same recommendations. Your maximum milk supply will mostly depend on where the cut was made, the breast mass removed (for reductions), and the time between your surgery and now. Breastfeeding consultants will work with you to get your best milk supply.
#6 – Will I be able to meet with a breastfeeding consultant?
Yes! Just ask your nurse to contact us, and we will be happy to help.
#7 – What if I can’t or choose not to breastfeed? What if I don’t have enough breastmilk?
We are here to support you and your baby in the NICU. You and your baby’s NICU team will decide what milk or combination of milk is best for your baby. We have different kinds of formula in the NICU to meet your baby’s nutritional needs. Some babies in the NICU also qualify for Pasteurized Human Milk (PHM) which is breastmilk that has been donated by other mothers in Quebec. The donor mothers are tested for infection, and their breastmilk is screened and pasteurized. Talk to your NICU team to learn more.
