
Celebrating Critical Care Transport Nurses at the MCH
18 February 2026
Rise in respiratory infections and measles outbreak: important infection prevention measures at the Montreal Children’s Hospital.
Read moreWelcome to the Montreal Children's Hospital

26 October 2016
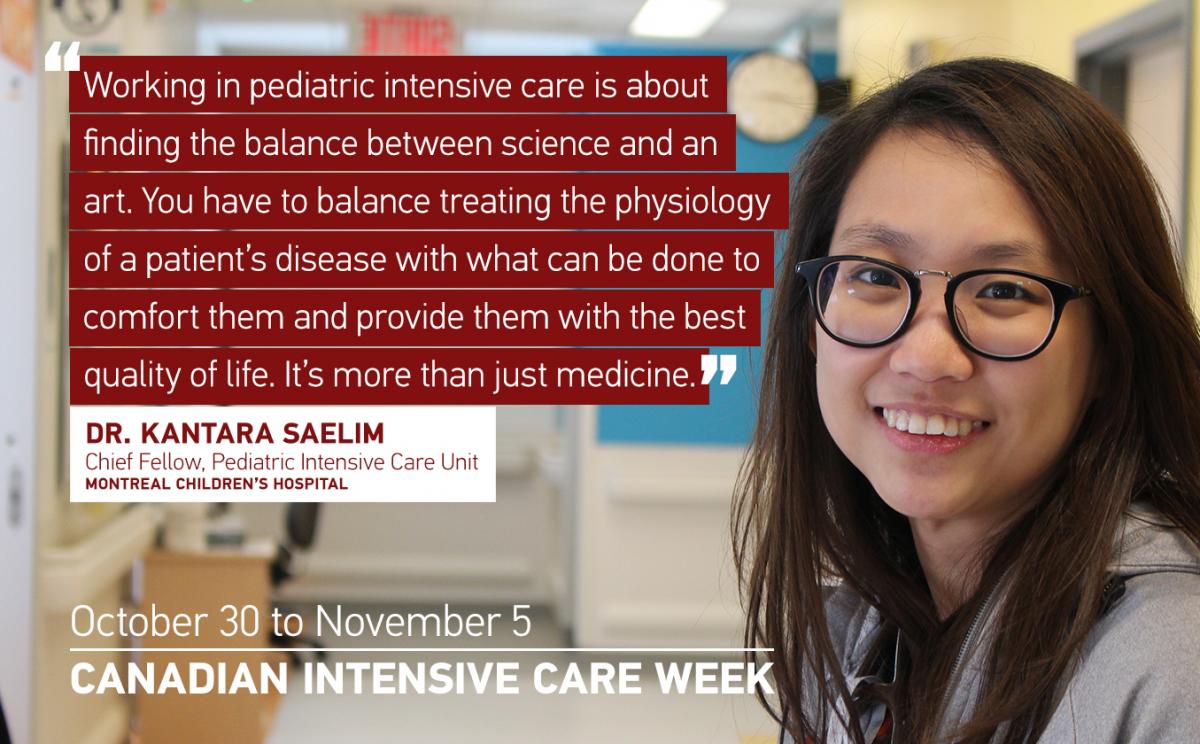
Dr. Kantara Saelim has always had her sights set on becoming a Pediatric Intensive Care Unit (PICU) Specialist. “I think I have the kind of personality for this work,” she explains. “I like staying challenged and busy, I never really stay still!” Kantara relocated from her native Thailand to complete additional specialized training (known as a pediatric fellowship) after having obtaining her medical degree and completing her residency in respirology in her home country. As a 2nd year fellow in the PICU at the Children’s, she is responsible for the care of patients in the unit all aged between infancy and 18 years old, all while managing the unit’s resources as efficiently as possible. “That’s the challenge of ICU care,” she explains. “You have to make fast, efficient and accurate decisions, and learn how to adjust your actions based on the priorities of your patients.”
The greatest difference between working in Canada versus Thailand – despite the much colder temperatures – is the multidisciplinary approach to patient care, says Kantara. “In Thailand, the team is made up of a physician and a nurse, whereas the approach here is much more specialized. You have a nutritionist, social worker, respiratory therapist, all working together with a physician and a nurse…in terms of patient care it’s a lot more interesting,” she explains.
The beauty of Kantara’s role, she says, lies in her quest to provide balanced, holistic care care to patients and families. “Unfortunately, not all patients go home in our unit,” she says. “The challenge is to not only think in terms of curable diseases, because sometimes there are no medical cures. Working in pediatric intensive care is about finding the balance between science and an art. You have to balance treating the physiology of a patient’s disease with what can be done to comfort them and provide them the best quality of life. It’s more than just medicine.”

“My first time ever examining a premature baby, I was a 3rd year medical student,” says Dr. Alicia Lambrinakos-Raymond, a 2nd year fellow in the Neonatal Intensive Care Unit (NICU) at the Montreal Children’s Hospital.“I remember feeling terrified that I would break the baby…I laugh at myself about it now!” Since that time, Alicia has cared for hundreds of premature infants – some as tiny as 500 grams –from the time they are born until they grow strong enough to go home, and is now completing highly specialized training in neonatology to become a NICU specialist.
“I wasn’t really sure what specialization I would pursue when I was completing my residency in pediatrics,” Alicia explains. “But asI spent more time in the NICU, I found that I really enjoyed the intensive nature of the work, how you have to act fast and make quick decisions.” Another aspect Alicia enjoys is building therapeutic relationships with parents, who often feel helpless when they first arrive in the unit. “I’ve learned that sometimes silence is golden when I first meet a family,” she says. “This is a very pivotal moment in time for them, and they are looking for ways to be included. I try to focus on what they can do to help their child during their hospitalization, so that they don’t feel like they are just bystanders but are empowered to do little things that can have a very big impact on their child’s health.”
The most satisfying part of her role, says Alicia, is being able to witness just how much her patients can grow and progress over time. “Sometimes small battles are really big gains for tiny patients,” she says, adding that it’s important to celebrate these positive milestones. “The greatest moment is watching the expression on a parent’s face as they leave the hospital with their baby, who is now well enough to go home in a car seat. It’s unbelievably rewarding.”