
Celebrating Critical Care Transport Nurses at the MCH
18 February 2026
Rise in respiratory infections and measles outbreak: important infection prevention measures at the Montreal Children’s Hospital.
Read moreWelcome to the Montreal Children's Hospital
28 August 2018
On the Pediatric Intensive Care Unit (PICU) at the Montreal Children’s Hospital, one patient can be under the care of several nurses, physicians and allied health professionals, each of whom has an essential role in carrying out the patient plan. With so many team members working at various points throughout the day and evening, an accurate handover of information is essential to delivering safe patient care. According to Dr. Samara Zavalkoff, an intensivist on the unit, “It’s an issue we’ve been looking at for some time and we needed a straightforward way to communicate the patient plan so that everyone had a clear understanding.”
The writing is on the window
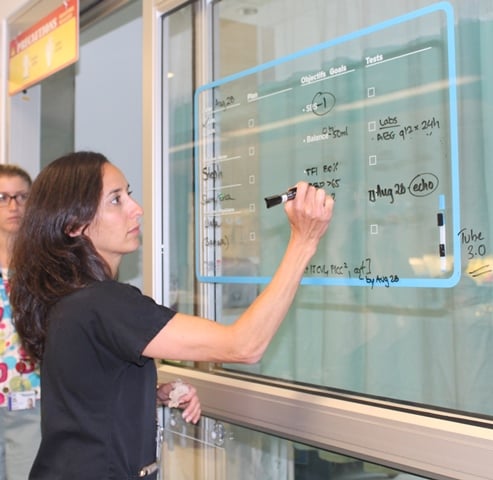
Inspired by an American hospital that used the walls in patient rooms to write down information, Dr. Zavalkoff saw an opportunity to be proactive and the Glass Door Project was launched. With the support of a multidisciplinary project team, which included two patient representatives, the group set specific, measurable, attainable, realistic, and timely (SMART) objectives and launched a pilot version of the project a little over a year ago. The idea is that an ICU team member writes the patient’s care plan on the glass door of the patient room. This can include, for example, goals for the patient’s blood pressure, a special test they need that day or a plan of when to start feeding. Each time an item is completed, staff check it off on the door, so that other team members can easily see the next steps to be completed.
This straightforward solution was met with some concerns however; there were worries about patient confidentiality and how consistent staff would be in writing everything down. “By starting slowly, and starting the project on only one patient room door, we were able to address issues as they came up and adjust the plan accordingly,” explains Dr. Zavalkoff. The patient confidentiality issue was addressed in collaboration with the Children’s ethicist, Lori Seller and certain steps were taken, like never writing the patient’s name or diagnosis on the door, to respect patient confidentiality. The percentage of staff who said they had a full understanding of the plan for their patient rose from 59% to 85% over a six month span and in term of usage, in the same amount of time, 96.7% of the doors were filled.
A survey of the entire unit showed that the top perceived benefits of the project are improved communication, that it’s easier to undertake tasks that consultants (who are not part of the PICU team but see the patients) know the plan, increased patient safety, improved infection control, and that families feel reassured. A secondary, yet very rewarding benefit is that parents feel more in the loop too. The project has since been implemented throughout the PICU, and steps are being taken to also implement the project on the Acute Care Unit (ACU).